Sequential Treatment of Schizophrenia – Interactive Case Study
Sequential treatment of schizophrenia helps psychiatrists clarify the stage of the patient's treatment and how to further guide pharmacotherapy. The following case study illustrates the possibilities for reducing negative and cognitive symptoms of schizophrenia while adhering to a metabolically sparing treatment approach.
Introduction
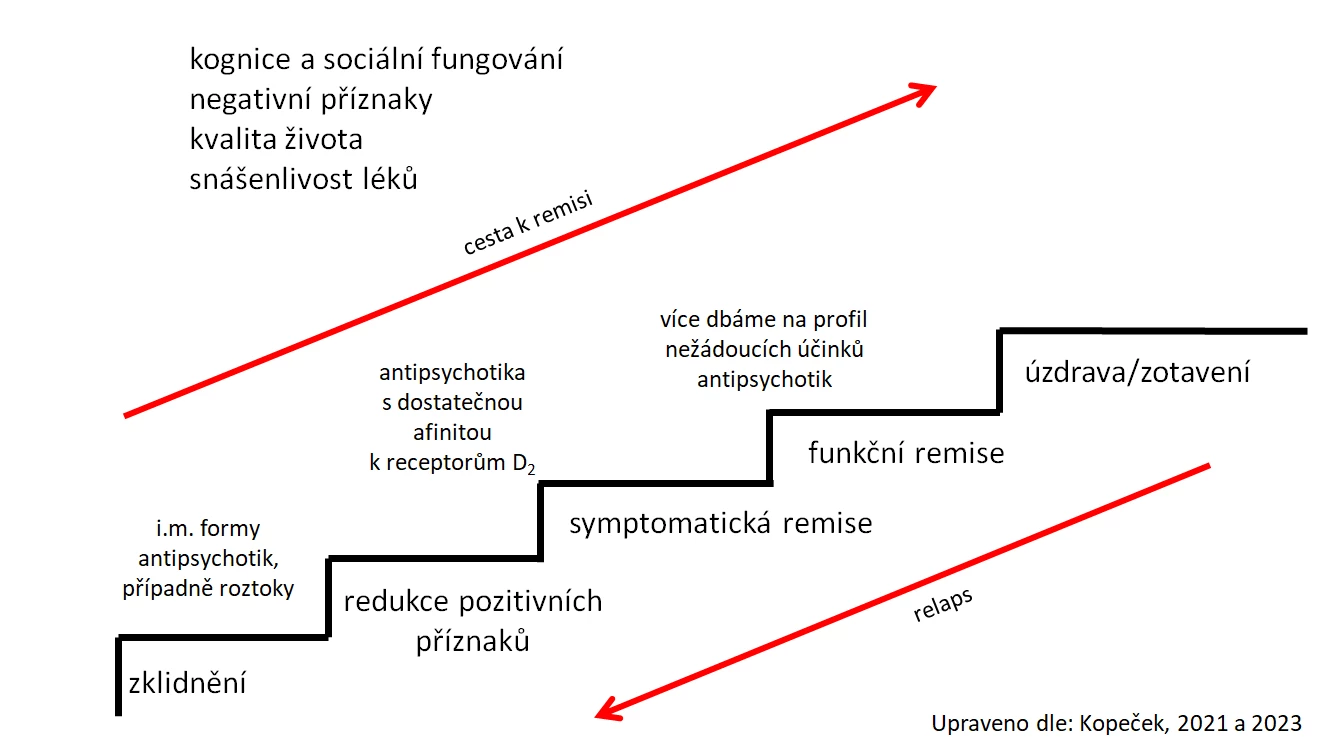
Sequential treatment of schizophrenia (see figure) is a method by which a clinical specialist in psychiatry can not only didactically illustrate and plan the treatment of an ill person, but also become aware of unmet needs in the treatment of patients with schizophrenia and plan their clinical interventions accordingly. Among the currently less or unmet needs in treatment, we can include the improvement of cognition and social functioning, the minimization of negative symptoms, and the improvement of quality of life - all with the long-term good tolerability of antipsychotics (Kopeček et al., 2021).
Medical History
The patient first presented for psychiatric evaluation at the age of 18. He described that between the ages of 12 and 16, he occasionally self-harmed by scratching his forearms with his nails during periods of increased stress at school. Between the ages of 16 and 17, he tried methamphetamine by snorting and marijuana by smoking several times. Since the age of 16, he has occasionally heard the voices of physically absent people commenting on his actions. His brother has been treated for paranoid schizophrenia since the age of 17. The other family members are mentally and physically healthy.
He himself has only been operated on once, for appendicitis. He has no other physical ailments and has no allergies. He has never had a head injury or been treated for epilepsy.
He has non-conflictual relationships with his parents and brother. His academic performance in elementary school was rather below average. He is currently studying at a vocational school. In the past year, he has not been interested in any hobbies and prefers to be alone. He has not yet sought intimate relationships. He does not have a driver's license.
Current Illness
In the past 9 months, he has been hearing the voices of strangers commenting on his thoughts and actions. Sometimes there is only one voice, but occasionally he hears multiple voices talking among themselves. If he listens to louder music or puts on headphones with music, he does not perceive these voices.
He feels anxious in environments with strangers. He sometimes feels that people walking by his residence stop under his apartment window to listen to his thoughts. He is convinced that others know what he is thinking. He thinks that people can take thoughts out of his head, leaving him unsure of what he was thinking. He fears that others are harming him this way. These feelings occur more often when he leaves home, such as for shopping, so he has been trying not to go out much lately. In the last month, he has not been able to attend school due to this reason.
At times, he fears that someone is tampering with his food and does not rule out the possibility that someone is trying to poison him. This leads to a reduced intake of food.
Examination
Objectively, auditory hallucinations were present, and hallucinatory behavior with listening was observed, as the patient would turn towards the hallucinated voices. He would sometimes cover his ears with large headphones. Intrapsychic hallucinations of thought withdrawal were also present. Paranoid-persecutory delusions were evident. The patient's thinking was incoherent with thought blocking. He was occasionally anxious, and his emotional reactivity was blunted. The patient's reported intrapsychic tension was reflected in his psychomotor agitation, as he would often get up and walk around the consultation room during the examination. Anhedonia was present. The patient's volitional activity was reduced, and his sleep was interrupted by repeated awakenings. Attention was decreased, and both short-term and long-term memory were impaired.
A native CT scan of the brain was performed - no pathological findings were observed. An EEG showed no grafoelements indicative of epilepsy. Toxicology tests of serum and urine excluded the presence of psychoactive substances. Parents' heteroanamnesis confirmed the symptoms and behavioral changes described by the patient and excluded the use of psychoactive substances by the patient. Social withdrawal was also evident from the heteroanamnesis, indicating that the patient had lost interest in contact with friends and classmates. Available information and examinations allowed for the diagnosis of paranoid schizophrenia.
The patient's BMI was 29.6, blood pressure (BP) 149/90 mmHg, and heart rate (HR) 122/min.
Initial Treatment
The patient was admitted to the hospital, and in the first few days, olanzapine was gradually increased to a dose of 20 mg daily. This led to the resolution of psychomotor agitation and anxiety and the normalization of sleep. Hallucinations and delusions, as well as emotional blunting, gradually reduced.
The patient no longer feared contact with strangers and would go outside during hospital passes. His appetite significantly improved. Hypobulia, anhedonia, and social withdrawal persisted, along with hypoprosexia and impairments in both short-term and long-term memory, with no significant change since the beginning of hospitalization. BMI increased to 30.2, BP improved to 135/85 mmHg, and HR to 85/min.
Conclusion
Olanzapine was subsequently cross-switched to lurasidone at a dose of 111 mg daily. The patient tolerated the treatment well, and his attention, as well as short-term and long-term memory, gradually improved. Emotional blunting subsided, and the patient showed increased interest in contact with family members and classmates. Body weight decreased, and BMI dropped to 29.8. He was discharged home in a slowly emerging functional remission. After 4 weeks of home treatment, he was able to return to school and continue his secondary education.
MUDr. Jan Hubeňák, Ph.D.
Psychiatric Clinic of the Faculty of Medicine, Charles University and University Hospital Hradec Králové
Did you like this article? Would you like to comment on it? Write to us. We are interested in your opinion. We will not publish it, but we will gladly answer you.
